--Lewis Carroll, Alice In Wonderland
And so, on to the final chapter of the story. Well, I am hoping this will be the final chapter.
BEFORE
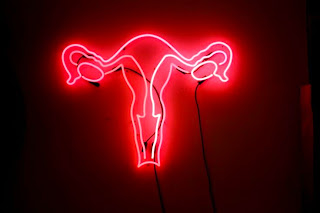
My pre-surgery appointment was
scheduled for Wednesday, May 27 at 10 AM. Kia Prescott, Dr. Muto’s Physician
Assistant, went over the particulars: this would be a complete hysterectomy,
removing the uterus, fallopian tubes and ovaries. (By now I had given up on my
crusade to retain my ovaries. Dr. Muto had reasoned that at this point in my
life, my ovaries excrete nothing.
Zilch. Nada. Zero. “If you were 39 years old, there would be a reason to debate
this. But not at 63.”) Kia’s main focus was the aftermath of the operation.
“You’re going to be tired for at least 6 weeks. Listen to what your body is
telling you. Don’t lift anything heavy. Rest. Take naps. You will not be able
to run around because you will hit the wall and come to a crashing halt. And
when I say hit the wall, I mean
you’ll have no reserves.” She delivered all of this forthrightly and
cheerfully, patiently enduring my repeated assertions about being as strong as
an ox. I bounce back from everything in record time, I insisted. “You’ll see,
you’re going to be a hot mess,” she smiled sweetly.
This was followed by a brief
conversation with the anesthesiologist. I repeated what I always say when meeting
an anesthesiologist, “No ketamine.” The
doctor assured me that ketamine was no longer used on human beings. (“It’s only
been used on horses for years!”) But on the subject of ketamine, my motto is Better Safe Than Sorry. I’d experienced
it 30 years ago when New York Hospital reset my broken nose, and life became an endless screening of the Sorcerer’s
Apprentice for the next several months.
 |
| Ketamine's aftermath |
With the anesthesiologist’s guarantee that ketamine was off the table, and armed with instructions to call and confirm my surgery appointment for noon the next day, we went to Boston’s Museum of Fine Arts to spend the afternoon.
 |
| John Singer Sargent paints sparkling white linen like no one else in this world. |
 |
| zzzzZZZZZZZZ |
Prepping for surgery is a little
like watching your life pass before your eyes. Only in this case, it’s not your
life's story crossing your field of vision, but an entire surgical team that comes
through, introducing itself one by one, asking if you know why you’re here, what
kind of surgery you’re expecting to have done, and if any of your teeth are
loose. (Again with the teeth?!) One member
of the team was a standout—Dominick, the anesthesiologist nurse. I wish I’d
asked his last name, because he was wonderful. Dominick took the time to
explain every move that would take place once I was in the operating room,
walking me through everything I would observe before falling asleep. This was
obviously done for the benefit of nervous patients, and it was the absolutely
perfect touch. The explanation included everything from how I would be moved from the
gurney to the operating table, to the moment when he would cease speaking to me
and turn to the surgical team to give them a status update.
The last thing I
recall before the lights went out was Dominick patting my shoulder, assuring me
that he would take good care of me, and promising me that I wouldn’t wake up
during the surgery. It hadn’t even occurred to me that this could happen. Hmmm, now that's a |
| Now that's a party hat. |
AFTER
I awoke to Peter’s and my brother,
Steve’s smiling faces. The recovery room was bustling beyond my pleasant haze
of drugs. I was offered vanilla pudding in a tiny dixie cup. I ate it with
drug-sodden gusto and was reduced to a gaga bleating of Oliver Twist’s, May I have some more, please? For the
time being, the usual zzZZZZZ had been reduced to hmmmmmm.
Steve, had come up from New York to
be with me. Over the years, Steve and I have made it a practice to sit with and
for each other during surgeries. Steve kept me company while Peter underwent back
surgeries. I sat with him while his wife, Susan, had surgery. We’ve never
discussed why or how this tradition came to be. As children, Steve and I fought endlessly. (I used to say that my
brother never spoke a civil word to me until I went off to college.) In a quiet
moment my mother took me aside and told me we shouldn’t fight because someday
she and my father would be gone, and Steve and I would have only each other.
 |
| Steve Doloff |
Somehow I got dressed. Peter must have made that happen. I was still so gaga
that I could easily have pulled my panties on over my yoga pants and thought I was ready to go dancing. I was poured into a wheelchair and rolled out of the hospital.
Although our hotel was two blocks from the hospital, Peter brought the car
around to pick me up. Steve stood beside me holding my hand, while I sat in the
wheelchair, blissed out, dreamy and secure in my brother’s company and care.
The hospital sent me home with scrip’s for big honkin’ bottles of 600 mg Ibuprofen and OxyCodone. The amount and magnitude of the medications seemed vastly out of line with the minor discomfort I was experiencing. True, urinating did sting for the next day or so, and I did feel like my bladder had been neatly folded in quarters, and then unfolded and refolded a few more times. (Having your hooha clamped wide open for almost two hours and your organs moved around like chops on a grill will have that effect.) But over-the-counter Advil would have done the trick.
The hospital sent me home with scrip’s for big honkin’ bottles of 600 mg Ibuprofen and OxyCodone. The amount and magnitude of the medications seemed vastly out of line with the minor discomfort I was experiencing. True, urinating did sting for the next day or so, and I did feel like my bladder had been neatly folded in quarters, and then unfolded and refolded a few more times. (Having your hooha clamped wide open for almost two hours and your organs moved around like chops on a grill will have that effect.) But over-the-counter Advil would have done the trick.
AFTER AFTER
Life is an elaborate and endless to-do list, and I plan my own life with bullet-points, indented sections and
subsections. But the list was put aside for the next
several weeks. I slept a great deal, I ate a very little, and somehow the time
passed hazily, pleasantly and uneventfully. The mild soreness passed, the fatigue that
Kia predicted did overcome me in many small ways over many late spring
afternoons. Amazingly, I was smart enough not to over-exert myself, so I never
did live out her prediction of becoming a hot mess. The lethargy was so pleasant, in fact, that I wondered if I would ever get beyond it. I missed the habitual zzzzzzzzz in my head, and asked myself, What happens if it doesn't come back, and I'm stuck in hmmmmm for the rest of my life? I needn't have worried. It came back with a vengeance (albeit, in fits and starts), and I am happily making and checking off long to-do lists again.
The pathology report was a howling success. The cancer was confirmed to be early, slow growing, and making only minor inroads into the muscle. Even better, the genetic testing showed no
inherent predisposition to the cancer. As Dr. Muto termed it, This was just a lightning strike.
And so we move forward. I dodged a bullet this time, and am immensely
grateful and relieved to have done so. But my blithe certainty of many
healthy years ahead is rightfully shaken. And the fragility of life and its
tender connections to beloved husbands, brothers, friends and memories are spread out before me plainly, just as they were when my mother and father died.